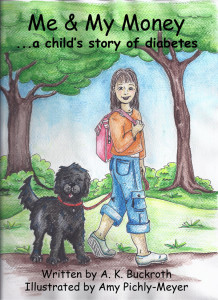
Copyrighted in 2012, Me & My Money…a child’s story of diabetes, took two years to write…
From birthing thoughts, jotting ideas, typing a manuscript, carrying a daily journal, contacting an illustrator, building the manuscript, proofreading and editing again and again and again and…you get the idea…this dream came to fruition. It had do be done. There is no other book like it — as far as my research goes — that reflects, mimics, or encourages diabetic children, T1Ds. The book is now available to the general public in paperback form. Celebrate!!
Submitting to a marketable world with a targeted audience, networking, promoting, speaking, through the main character, Kali with her dog, Money, brings attention to the increase of diabetes in animals – up 300% this past decade!
Through the wonderful insightfulness of illustrator Amy Pichly-Meyer who is responsible for the clarity of expression with the cover design, along with all 37 colored illustrations, this book was built for you. I am thankful for her friendship and abilities.
Briefly, the main character, Kali, is presently a fourth grader. She was diagnosed with diabetes at the age of two. Her rapid growth with blooming and wizened independence results from learning how to take care of herself. Wayne, a best friend, knows her very well and together they embark on adventures through Wayne’s hobby, their separate and shared responsibilities, mutual friends, and more. But Kali cannot forget her special pack! She must carry this with her everyday, everywhere.
This book, along with the recent publication of Me & My Money Too…a child’s story with diabetes, are tools to understanding this disease. Minute-by-minute self-care is introduced and forthcoming in this illustrated, easy-to-read chapter book, 104 pages long, appropriate for 8 years olds and available at Amazon.com in paperback edition as well as Kindle e-readers. Local bookstores carry copies as well as local libraries with requests. Please enjoy the following Chapter excerpts…
Chapter 1, Book One
Due to keeping up with my chores, I occasionally have some change in my pocket. That’s because my parents give me a weekly allowance that I can spend when I want.
“Make sure you spend wisely,’ Dad says. I’m not quite sure what “spend wisely” means, but I think I do okay with what I have. For instance, one of my friends from school, Wayne, asked me to go to the hobby store one Saturday afternoon. Because it is school summer vacation time, we could go almost any time, depending on our parents. However, Saturday’s are best.
Wayne and I go way back, to kindergarten. He is the only red-head kid in our whole grammar school, never mind our fourth grade. He’s a full blown carrot top with thick hair in wavy curls. This makes him real easy to spot in a crowd. The girls in our class like Wayne more than the boys do. I think this is because he has good manners and is polite. It is either that or his clear sky blue eyes that sparkle. Even his eyelashes are orange, matching his hair. Most girls I know like blue eyes. I never thought about it much. My eyes are dark brown to match my light brown and blonde streaky hair.
Wayne is a pale looking kid. Most of the time, the only color on Wayne’s face is because of his tannish-brown colored freckles. I swear, if he didn’t have freckles, he would be white as a ghost! I tease him about that, pretending that I can’t see him sometimes. We laugh. He blushes all red and pink. It’s funny to see. Wayne is shorter than I am — for now. He teases me about my long brown hair — so flat, so straight and thin. “There’s nothing to your hair,” he tells me as he quickly flicks it in the air. “You don’t even have to brush it. Your hair just hangs there off your fat head,” he often tells me as if I need to be reminded.
I think Wayne is jealous of my straight hair. Brushing his hair is a struggle because it is very thick. Mine is a lot easier because it is stick straight. He hates when his mother brushes his hair because “she always pulls it out of my head,” he told me one time. “And you have a chubby little pug-nose. Not like my pointy one at all,” he compares. “But you get a tan in the summer. I don’t tan, I burn. It’s awful,” he explains. That is true.
One summer that I remember, his mother covered his face and arms with white suntan lotion so he wouldn’t get burned while playing with me in my back yard. He looked so funny. That stuff made him smell like the beach. I laughed at him. He didn’t like that. And after a while, the suntan lotion disappeared. But we stayed friends. He wears that stuff all the time. Sure, I use it too, but when I forget to rub it on my skin, I don’t get too worried.
“I guess you look like your father,” I told him because I think he does. “I look like my mother,” I said. And that’s okay with me because my mother is beautiful. My Dad’s okay looking — for a Dad. Sometimes he has a moustache. Mom told him to shave it off because it made her sneeze when they kiss. Eeeuu! Sneezing and kissing, yuck!
“Kali,” my mom called up the stairs. “Wayne is on the phone for you.”
“Okay. Thanks. I’ll get it up here,” I told her.
“Hi Wayne. Wassup?”
“Hey. Can you come to the train store with me today or what? I’m looking for a certain model train engine and I think the Viking Hobby Store will have it.”
Well, I have no particular interest in model trains, so I knew I wouldn’t buy anything but I would go along with him anyway. This is a wise decision. After all, he is my very best friend. Very best friends do things for each other whether we need to or like to or not. It was Saturday morning anyway. Cleaning my room could wait until I got back. I was thinking, planning.
“Mom, Dad, is it okay with you if I go to the hoppy store with Wayne today? He thinks he found the perfect train engine for his set. He wants me to go and help him check it out.”
“I don’t mind. Is your room picked up?” Mom asked.
“Not all the way yet, Mom,” I replied. “I can finish when I get back. All I have to do is fold my clothes and put them away. A load of my socks and some t-shirts are still in the dryer.”
“Well, all right. Did you ask your father?” Mom wanted to know. “And don’t forget to take a snack and some juice boxes with you.”
“I know. I already have a pack of peanut butter nabs in my sack with some water. I don’t know where Dad is. I thought he was in the kitchen with you. Maybe he’s in the garage.”
“Okay,” continued my mother. “If you don’t see your father on your way out, I’ll tell him. If you do, please remind him that we’re going shopping today. Oh, are you and Wayne taking your bikes or walking?”
“I think we’ll walk.” And out the back door I went.
Chapter 2
Wayne lives four houses away from me. I took the short-cut over to his house through a wildflower field. I often come here to pick my mother some flowers. I like to pick flowers for her. There are all kinds of wildflowers in this field: yellow ones, pink ones, purple ones with yellow centers. I don’t know the names of these flowers, I just know they are pretty and Mom likes them.
After I met Wayne on the front porch of his house, we proceeded to walk to this particular ‘train store’ as he calls it. It is really a hobby store that has lots of other things of interest besides trains. I’ve been in there with one of my older cousins. She was looking for some particular, special types of paint brushes made with camel’s hair. I thought that was cool — paint brushes made out of a camel’s hair! There are small glider planes in this store with hand-held motor devices; there are different kinds of wood burners and wood carving tools; there are even lots of different colored rubber fish bait things — lures. I liked those because they are shiny, squishy, and they squiggle. Things that would attract a fish — go figure! Wayne had been going on about a certain model train engine he saw in here a while ago. It took him weeks and weeks to save up his allowance money to buy it.
“Hey, before we walk too far, is your insulin pump filled up?” Wayne asked. “I hope it doesn’t beep like crazy while we are out. I would hate to have to leave early so you could fix it.”
“Yes, it’s fine. I filled it up with insulin yesterday morning and changed the needle site. We are good to go!” I planned this on purpose. I knew he would ask. I am diabetic. Wayne knows. Among many other things, I do take care of myself and my diabetes. I have to test my blood sugar levels many times each day. Diabetes is a disease that causes me not to digest food properly. Because of that, I wear an insulin pump. I used to have to take insulin shots before I got the pump. Having the pump is much easier. An insulin pump squirts insulin into my body, automatically, a tiny bit at a time. A “squirt” is maybe the size of a pencil tip or the size of a period at the end of a sentence. My parents had to give me insulin shots before I learned to give them myself. I still keep syringes handy, in case the pump breaks down for whatever reason. This is called having “Plan B” which is important.
Read more of Kali’s young life with diabetes in “Me & My Money…a child’s story of diabetes.” Available at Amazon.com.